Testicular Cancer Treatment
Testicular Cancer
What is Testicular Cancer?
Testicular cancer is a relatively rare type of cancer that develops in the testicles — the male reproductive glands located within the scrotum, a loose sac of skin beneath the penis. The testicles produce testosterone and sperm and are vital for male fertility and hormonal balance.
Most cases of testicular cancer begin in the germ cells, which are responsible for producing sperm.
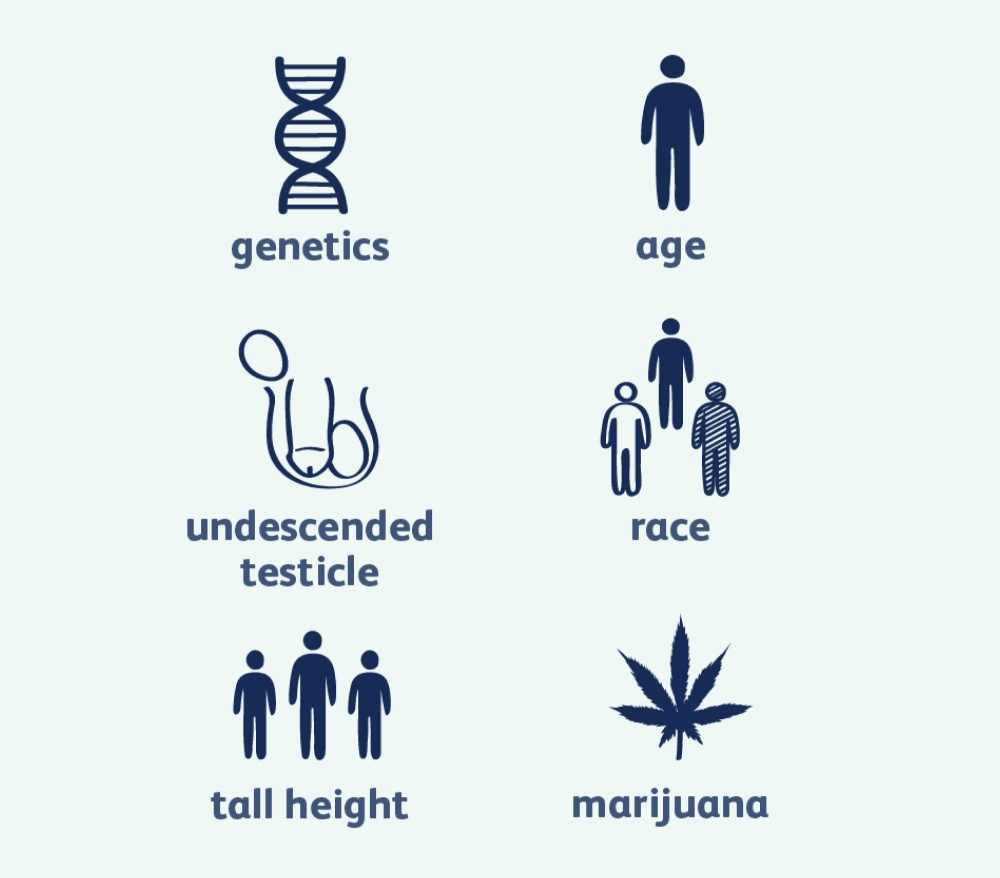
Causes & Risk Factors of Testicular Cancer
While the exact cause is unknown, several risk factors may increase the likelihood of developing testicular cancer:
- Undescended testicle (Cryptorchidism)
- Abnormal testicular development (e.g., Klinefelter syndrome)
- Family history of testicular cancer
- Age (Most common in men between 15–35 years )
- Previous testicular cancer
- Infertility
- HIV infection
Types of Testicular Cancer
- Germ Cell Tumours (GCTs)
Accounting for over 90% of testicular cancers, GCTs originate from sperm-producing cells. They are classified into:
- Seminomas: Slow-growing and highly responsive to radiation therapy. Often increase levels of the hormone HCG (Human Chorionic Gonadotropin).
- Subtypes: Classical seminomas, Spermatocytic seminomas
- Non-seminomas: More aggressive and commonly affect younger men.
- Subtypes: Embryonal carcinoma, Yolk sac tumour, Choriocarcinoma, Teratoma
- Carcinoma In Situ (CIS)
Also called Intratubular Germ Cell Neoplasia, this is a non-invasive condition that can potentially develop into invasive cancer if not treated early.
- Stromal Tumours
These are rare and develop from the supportive tissue of the testicles.
- Leydig Cell Tumours
- Sertoli Cell Tumours
- Secondary Testicular Cancer
Cancers that start in other organs (like prostate or kidney) and metastasize to the testicles.
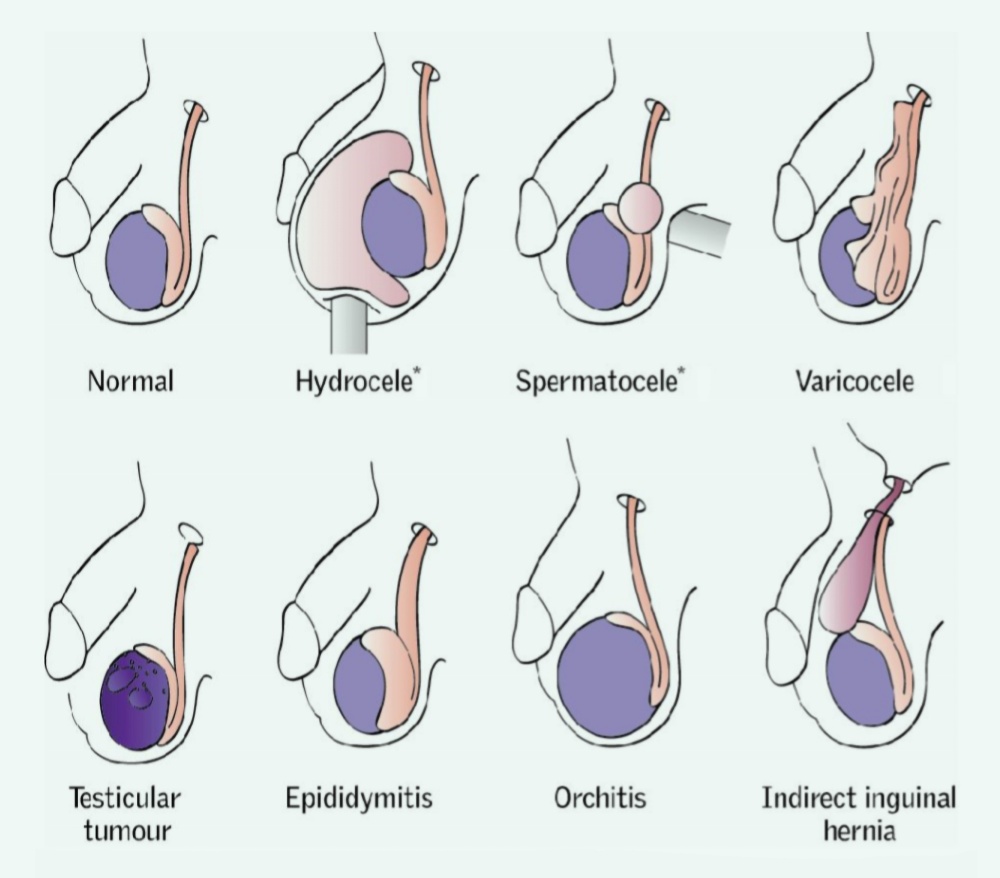
Symptoms of Testicular Cancer
Testicular cancer often presents with mild or painless symptoms in its early stages. Watch out for:

Lower back pain (in advanced cases)

Enlargement or firmness of the testicle

A dull ache or pain in the groin or lower abdomen

Sudden build-up of fluid in the scrotum

Feeling of heaviness in the scrotum

Discomfort or pain in the testicle or scrotum

A lump or swelling in either testicle

Can Testicular Cancer Be Prevented?
There is no guaranteed way to prevent testicular cancer. However, being aware of your body and performing regular testicular self-exams can help detect abnormalities early. Men at high risk (due to family history or undescended testicles) should consider regular screening.
How Testicular Cancer Is Diagnosed
- Physical Examination
A doctor checks for lumps, swelling, or changes in the size or firmness of the testicles.
- Medical & Family History Review
Helps identify inherited or lifestyle risk factors.
- Tumour Marker Blood Tests
- Certain proteins can be elevated in testicular cancer:
- Alpha-fetoprotein (AFP)
- Beta-Human Chorionic Gonadotropin (β-HCG)
- Lactate Dehydrogenase (LDH)
- Scrotal Ultrasound
Non-invasive imaging to examine any abnormal masses in the testicles.
- Inguinal Orchiectomy (Surgical Biopsy)
The affected testicle is surgically removed and examined to confirm the type of cancer.
- Additional Imaging Tests
- CT Scan
- X-ray
- MRI or PET Scan – To check for cancer spread (metastasis)

Treatment Options for Testicular Cancer
Treatment depends on the type, stage of the disease, and overall health of the patient. Most testicular cancers are highly treatable, even in advanced stages.
- Radical Inguinal Orchiectomy: Removal of the affected testicle.
- Retroperitoneal Lymph Node Dissection (RPLND): Removal of nearby lymph nodes to prevent cancer spread.
Often used to treat seminomas. High-energy rays are targeted at cancer cells either externally or internally (brachytherapy).
Drugs are used to destroy cancer cells throughout the body. Administered orally or intravenously. Effective against non-seminomas and advanced-stage cancers.
Used in recurrent or resistant cases. Damaged bone marrow is replaced using stem cells after intense chemotherapy.




