Vulval Cancer Treatment
Vulval cancer

Vulval cancer care at Thangam cancer center
Vulval cancer is a rare form of cancer that affects the external female genitalia, collectively known as the vulva. This includes the labia majora, labia minora, clitoris, mons pubis, vaginal opening, and urethral opening. Vulval cancer accounts for approximately 4% of all gynaecological cancers and is most commonly seen in older women.
At Thangam Hospital, our expert gynaecologic oncology team specializes in diagnosing and treating vulval cancer with compassion and precision, offering advanced treatments including minimally invasive and robotic surgery.
Causes and Risk Factors of Vulval Cancer
While the exact cause is not always clear, several risk factors have been identified:
Age
Most cases occur in women over 70 years old.
HPV Infection
Persistent infection with Human Papillomavirus (especially HPV-16) increases risk.
VIN (Vulvar Intraepithelial Neoplasia)
A known precursor to vulval cancer.
Lichen Sclerosis
A chronic skin condition, especially in postmenopausal women, that raises the risk of squamous cell carcinoma.
Smoking
Smoking weakens immune defenses and increases cancer risk.
Immunosuppression
Women with HIV or those on immunosuppressant therapy (e.g., post-transplant) have a higher risk.
Symptoms of Vulval Cancer
Early detection of vulval cancer significantly improves treatment outcomes. Look out for the following symptoms:

Persistent itching or burning in the vulval region

Pain or discomfort while urinating

Bleeding or pain during or after sexual intercourse

Swelling, discoloration, or ulcers on the vulva

Lump, sore, or wart-like growth in the vulval or groin area
If these symptoms last more than two weeks, consult a gynaecologic oncologist immediately.
Types of Vulval Cancer
- Squamous Cell Carcinoma
This is the most common type, making up around 90% of vulval cancer cases. It often develops from a precancerous condition called Vulvar Intraepithelial Neoplasia (VIN). It may be associated with persistent HPV infection or conditions like vulvar dystrophy, especially in older women.
Verrucous carcinoma is a rare, slow-growing subtype with a wart-like appearance.
- Vulvar Melanoma
This type accounts for about 5% of vulval cancers. It typically presents as a dark or irregularly pigmented mole, but may also appear pink, red, or white. Any changes in existing moles on the vulva should be examined promptly.
- Adenocarcinoma
Originates in the glandular tissues of the vulva, often presenting as swelling or a non-healing sore.
- Sarcoma
An aggressive and rare cancer that develops in the connective tissues of the vulva.
- Vulvar Intraepithelial Neoplasia (VIN)
A precancerous condition that may lead to squamous cell carcinoma. VIN often causes chronic itching and visible skin changes such as thickening or discoloration. Because its symptoms can mimic non-cancerous skin conditions, it is often misdiagnosed or self-treated — delaying proper care.
Diagnosis of Vulval Cancer
At Thangam Hospital, we use a combination of clinical assessment and advanced diagnostic tools:
- Pelvic Examination: Physical inspection of the vulval and groin region
- Biopsy: A small tissue sample is taken from the affected area to confirm the diagnosis
- Colposcopy: A magnified visual examination of the vulva
- Imaging Tests (MRI, CT, PET-CT): To evaluate the extent of disease spread to lymph nodes or other organs
- Sentinel Lymph Node Biopsy: To assess cancer spread in early-stage cases
Treatment Options for Vulval Cancer
Treatment is personalized based on the type, size, location, and stage of the cancer. Our multidisciplinary team offers the following treatment approaches:
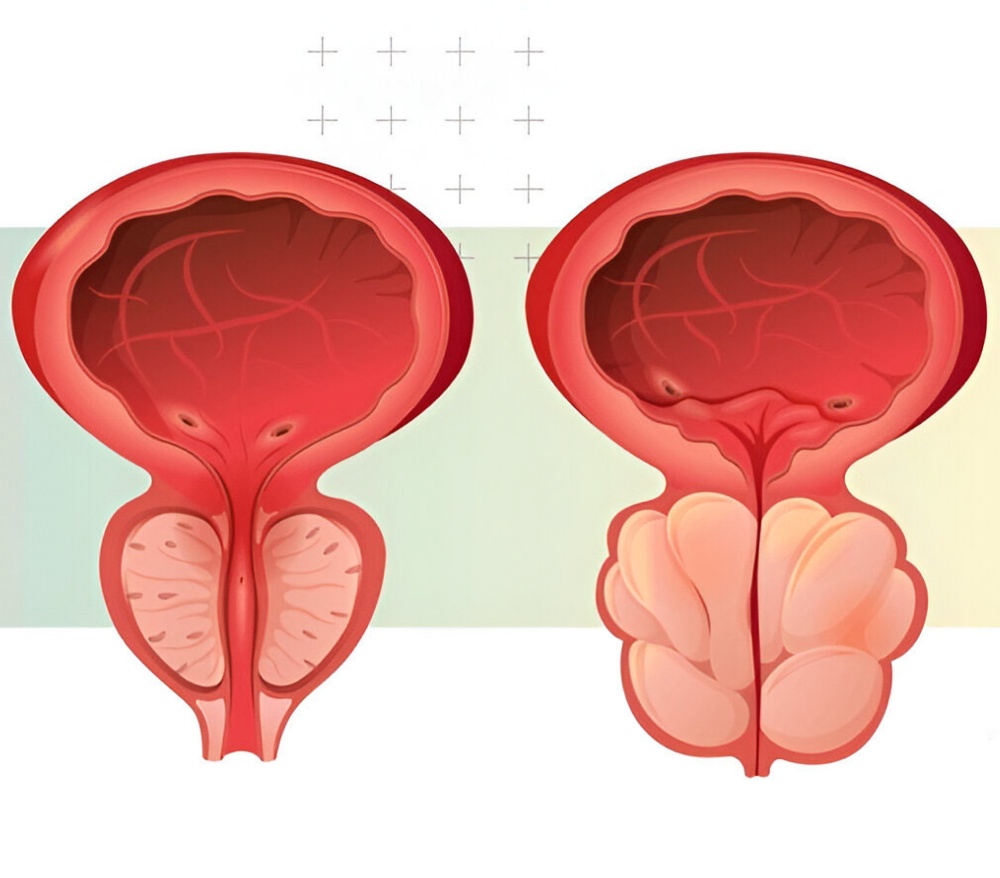
Surgery is the primary treatment for vulval cancer.
Wide Local Excision: Removal of the cancerous tissue with a margin of healthy tissue
Vulvectomy:
- Partial Vulvectomy: Only part of the vulva is removed
- Radical Vulvectomy: Complete removal of the vulva in more extensive cases
Lymph Node Dissection: Removal of lymph nodes in the groin to check for spread
Sentinel Lymph Node Mapping: A less invasive approach to detect early lymphatic spread
Minimally invasive and robotic-assisted surgical techniques may be used for improved recovery and reduced complications.
Radiation may be used:
- Before surgery (neoadjuvant) to shrink large tumors
- After surgery (adjuvant) to eliminate residual cancer cells
- As the primary treatment in patients who are not surgical candidates
Chemotherapy may be combined with radiation (chemoradiation) in advanced stages or for patients who are not suitable for surgery. It may also be used in recurrent or metastatic disease.
In selected cases, targeted therapies or immunotherapy may be used, particularly for advanced or recurrent vulval cancer, based on tumor markers and molecular testing.





